Recommended immunization schedule — original pdf
Backup
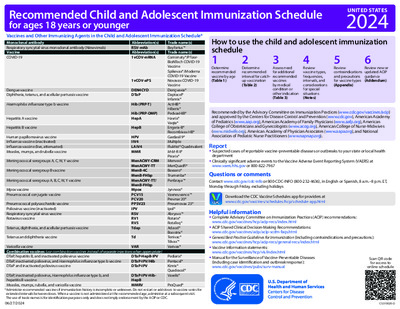
Recommended Child and Adolescent Immunization Schedule for ages 18 years or younger Vaccines and Other Immunizing Agents in the Child and Adolescent Immunization Schedule* Monoclonal antibody Respiratory syncytial virus monoclonal antibody (Nirsevimab) Vaccine COVID-19 Abbreviation(s) RSV-mAb Abbreviation(s) 1vCOV-mRNA UNITED STATES 2024 Dengue vaccine Diphtheria, tetanus, and acellular pertussis vaccine Haemophilus influenzae type b vaccine Hepatitis A vaccine Hepatitis B vaccine Human papillomavirus vaccine Influenza vaccine (inactivated) Influenza vaccine (live, attenuated) Measles, mumps, and rubella vaccine Meningococcal serogroups A, C, W, Y vaccine Meningococcal serogroup B vaccine Meningococcal serogroup A, B, C, W, Y vaccine Mpox vaccine Pneumococcal conjugate vaccine Pneumococcal polysaccharide vaccine Poliovirus vaccine (inactivated) Respiratory syncytial virus vaccine Rotavirus vaccine Tetanus, diphtheria, and acellular pertussis vaccine Tetanus and diphtheria vaccine How to use the child and adolescent immunization schedule 2 1 3 5 4 6 Determine recommended vaccine by age (Table 1) Determine recommended interval for catch- up vaccination (Table 2) Assess need for additional recommended vaccines by medical condition or other indication (Table 3) Review vaccine types, frequencies, intervals, and considerations for special situations (Notes) Review contraindications and precautions for vaccine types (Appendix) Review new or updated ACIP guidance (Addendum) Recommended by the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Control and Prevention (www.cdc.gov), American Academy of Pediatrics (www.aap.org), American Academy of Family Physicians (www.aafp.org), American College of Obstetricians and Gynecologists (www.acog.org), American College of Nurse-Midwives (www.midwife.org), American Academy of Physician Associates (www.aapa.org), and National Association of Pediatric Nurse Practitioners (www.napnap.org). Report y Suspected cases of reportable vaccine-preventable diseases or outbreaks to your state or local health department y Clinically significant adverse events to the Vaccine Adverse Event Reporting System (VAERS) at www.vaers.hhs.gov or 800-822-7967 Questions or comments Contact www.cdc.gov/cdc-info or 800-CDC-INFO (800-232-4636), in English or Spanish, 8 a.m.–8 p.m. ET, Monday through Friday, excluding holidays Download the CDC Vaccine Schedules app for providers at www.cdc.gov/vaccines/schedules/hcp/schedule-app.html Helpful information y Complete Advisory Committee on Immunization Practices (ACIP) recommendations: www.cdc.gov/vaccines/hcp/acip-recs/index.html y ACIP Shared Clinical Decision-Making Recommendations: www.cdc.gov/vaccines/acip/acip-scdm-faqs.html y General Best Practice Guidelines for Immunization (including contraindications and precautions): www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html 1vCOV-aPS DEN4CYD DTaP Hib (PRP-T) Hib (PRP-OMP) HepA HepB HPV IIV4 LAIV4 MMR MenACWY-CRM MenACWY-TT MenB-4C MenB-FHbp MenACWY-TT/ MenB-FHbp Mpox PCV15 PCV20 PPSV23 IPV RSV RV1 RV5 Tdap Td Trade name(s) Beyfortus™ Trade name(s) Comirnaty®/Pfizer- BioNTech COVID-19 Vaccine Spikevax®/Moderna COVID-19 Vaccine Novavax COVID-19 Vaccine Dengvaxia® Daptacel® Infanrix® ActHIB® Hiberix® PedvaxHIB® Havrix® Vaqta® Engerix-B® Recombivax HB® Gardasil 9® Multiple FluMist® Quadrivalent M-M-R II® Priorix® Menveo® MenQuadfi® Bexsero® Trumenba® Penbraya™ Jynneos® Vaxneuvance™ Prevnar 20® Pneumovax 23® Ipol® Abrysvo™ Rotarix® RotaTeq® Adacel® Boostrix® Tenivac® Tdvax™ Varivax® Pediarix® Pentacel® Kinrix® Quadracel® Vaxelis® Varicella vaccine Combination vaccines (use combination vaccines instead of separate injections when appropriate) DTaP, hepatitis B, and inactivated poliovirus vaccine DTaP, inactivated poliovirus, and Haemophilus influenzae type b vaccine DTaP and inactivated poliovirus vaccine DTaP-HepB-IPV DTaP-IPV/Hib DTaP-IPV VAR y Vaccine information statements: www.cdc.gov/vaccines/hcp/vis/index.html y Manual for the Surveillance of Vaccine-Preventable Diseases (including case identification and outbreak response): www.cdc.gov/vaccines/pubs/surv-manual DTaP, inactivated poliovirus, Haemophilus influenzae type b, and hepatitis B vaccine Measles, mumps, rubella, and varicella vaccine * Administer recommended vaccines if immunization history is incomplete or unknown. Do not restart or add doses to vaccine series for extended intervals between doses. When a vaccine is not administered at the recommended age, administer at a subsequent visit. The use of trade names is for identification purposes only and does not imply endorsement by the ACIP or CDC. 06/27/2024 DTaP-IPV-Hib- HepB MMRV ProQuad® Scan QR code for access to online schedule CS310020-D Table 1 Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 These recommendations must be read with the notes that follow. For those who fall behind or start late, provide catch-up vaccination at the earliest opportunity as indicated by the green bars. To determine minimum intervals between doses, see the catch-up schedule (Table 2). Vaccine and other immunizing agents Birth 1 mo 2 mos 4 mos 6 mos 9 mos 12 mos 15 mos 18 mos 19–23 mos 2–3 yrs 4–6 yrs 7–10 yrs 11–12 yrs 13–15 yrs 16 yrs 17–18 yrs Respiratory syncytial virus (RSV-mAb [Nirsevimab]) 1 dose depending on maternal RSV vaccination status, See Notes 1 dose (8 through 19 months), See Notes Hepatitis B (HepB) 1st dose ----- 2nd dose ----- ---------------------------- 3rd dose ---------------------------- Rotavirus (RV): RV1 (2-dose series), RV5 (3-dose series) Diphtheria, tetanus, acellular pertussis (DTaP <7 yrs) 1st dose 2nd dose See Notes 1st dose 2nd dose 3rd dose ----- 4th dose ------ 5th dose Haemophilus influenzae type b (Hib) 1st dose 2nd dose See Notes -- 3rd or 4th dose, -- See Notes 1st dose 2nd dose 3rd dose ----- 4th dose ----- COVID-19 (1vCOV-mRNA, 1vCOV-aPS) 1 or more doses of updated (2023–2024 Formula) vaccine (See Notes) 1st dose 2nd dose ---------------------------- 3rd dose ---------------------------- 4th dose See Notes Annual vaccination 1 or 2 doses Annual vaccination 1 dose only or Annual vaccination 1 or 2 doses Annual vaccination 1 dose only Measles, mumps, rubella (MMR) See Notes ----- 1st dose ----- ----- 1st dose ----- See Notes 2-dose series, See Notes 2nd dose 2nd dose See Notes 1 dose See Notes 1st dose 2nd dose See Notes Seasonal administration during pregnancy, See Notes Seropositive in endemic dengue areas (See Notes) Pneumococcal conjugate (PCV15, PCV20) Inactivated poliovirus (IPV <18 yrs) Influenza (IIV4) or Influenza (LAIV4) Varicella (VAR) Hepatitis A (HepA) Tetanus, diphtheria, acellular pertussis (Tdap ≥7 yrs) Human papillomavirus (HPV) Meningococcal (MenACWY-CRM ≥2 mos, MenACWY-TT ≥2years) Meningococcal B (MenB-4C, MenB-FHbp) Respiratory syncytial virus vaccine (RSV [Abrysvo]) Dengue (DEN4CYD; 9-16 yrs) Mpox Range of recommended ages for all children Range of recommended ages for catch-up vaccination Range of recommended ages for certain high-risk groups Recommended vaccination can begin in this age group Recommended vaccination based on shared clinical decision-making No recommendation/ not applicable Table 2 Recommended Catch-up Immunization Schedule for Children and Adolescents Who Start Late or Who Are More than 1 Month Behind, United States, 2024 The table below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child’s age. Always use this table in conjunction with Table 1 and the Notes that follow. Vaccine Hepatitis B Rotavirus Diphtheria, tetanus, and acellular pertussis Minimum Age for Dose 1 Birth Dose 1 to Dose 2 4 weeks 6 weeks Maximum age for first dose is 14 weeks, 6 days. 6 weeks 4 weeks 4 weeks Children age 4 months through 6 years Minimum Interval Between Doses Dose 2 to Dose 3 8 weeks and at least 16 weeks after first dose minimum age for the final dose is 24 weeks 4 weeks maximum age for final dose is 8 months, 0 days 4 weeks 6 months Dose 3 to Dose 4 Dose 4 to Dose 5 6 months A fifth dose is not necessary if the fourth dose was administered at age 4 years or older and at least 6 months after dose 3 Haemophilus influenzae type b 6 weeks Pneumococcal conjugate 6 weeks No further doses needed if first dose was administered at age 15 months or older. 4 weeks if first dose was administered before the 1st birthday. 8 weeks (as final dose) if first dose was administered at age 12 through 14 months. No further doses needed for healthy children if first dose was administered at age 24 months or older 4 weeks if first dose was administered before the 1st birthday 8 weeks (as final dose for healthy children) if first dose was administered at the 1st birthday or after No further doses needed if previous dose was administered at age 15 months or older 4 weeks if current age is younger than 12 months and first dose was administered at younger than age 7 months and at least 1 previous dose was PRP-T (ActHib®, Pentacel®, Hiberix®), Vaxelis® or unknown 8 weeks and age 12 through 59 months (as final dose) if current age is younger than 12 months and first dose was administered at age 7 through 11 months; OR if current age is 12 through 59 months and first dose was administered before the 1st birthday and second dose was administered at younger than 15 months; OR if both doses were PedvaxHIB® and were administered before the 1st birthday No further doses needed for healthy children if previous dose was administered at age 24 months or older 4 weeks if current age is younger than 12 months and previous dose was administered at <7 months old 8 weeks (as final dose for healthy children) if previous dose was administered between 7–11 months (wait until at least 12 months old); OR if current age is 12 months or older and at least 1 dose was administered before age 12 months 8 weeks (as final dose) This dose only necessary for children age 12 through 59 months who received 3 doses before the 1st birthday. 8 weeks (as final dose) This dose is only necessary for children age 12 through 59 months regardless of risk, or age 60 through 71 months with any risk, who received 3 doses before age 12 months. 6 months (minimum age 4 years for final dose) 4 weeks if current age is <4 years 6 months (as final dose) if current age is 4 years or older Inactivated poliovirus 6 weeks 4 weeks Measles, mumps, rubella Varicella Hepatitis A Meningococcal ACWY 12 months 12 months 12 months 2 months MenACWY-CRM 2 years MenACWY-TT 4 weeks 3 months 6 months 8 weeks Meningococcal ACWY Tetanus, diphtheria; tetanus, diphtheria, and acellular pertussis Not applicable (N/A) 7 years 8 weeks 4 weeks Human papillomavirus 9 years Hepatitis A Hepatitis B Inactivated poliovirus N/A N/A N/A Routine dosing intervals are recommended. 6 months 4 weeks 4 weeks Measles, mumps, rubella Varicella N/A N/A 4 weeks 3 months if younger than age 13 years. 4 weeks if age 13 years or older Dengue 9 years 6 months 6 months See Notes See Notes Children and adolescents age 7 through 18 years 4 weeks if first dose of DTaP/DT was administered before the 1st birthday 6 months (as final dose) if first dose of DTaP/DT or Tdap/Td was administered at or after the 1st birthday 6 months if first dose of DTaP/DT was administered before the 1st birthday 8 weeks and at least 16 weeks after first dose 6 months A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months after the previous dose. A fourth dose of IPV is indicated if all previous doses were administered at <4 years OR if the third dose was administered <6 months after the second dose. Table 3 Recommended Child and Adolescent Immunization Schedule by Medical Indication, United States, 2024 Always use this table in conjunction with Table 1 and the Notes that follow. Medical conditions are often not mutually exclusive. If multiple conditions are present, refer to guidance in all relevant columns. See Notes for medical conditions not listed. Pregnancy Immunocompromised (excluding HIV infection) 2nd RSV season HIV infection CD4 percentage and counta <15% or <200mm ≥15% and ≥200mm CSF leak or cochlear implant Asplenia or persistent complement component deficiencies Heart disease or chronic lung disease Chronic liver disease Diabetes Kidney failure, End-stage renal disease or on Dialysis 1 dose depending on maternal RSV vaccination status, See Notes 2nd RSV season for chronic lung disease (See Notes) 1 dose depending on maternal RSV vaccination status, See Notes DTaP Tdap: 1 dose each pregnancy SCIDb HSCT: 3 doses See Notes See Notes COVID-19 See Notes Asthma, wheezing: 2–4 yearsc 3 dose series. See Notes Vaccine and other immunizing agents RSV-mAb (nirsevimab) Hepatitis B Rotavirus DTaP/Tdap Pneumococcal Hib IPV IIV4 LAIV4 MMR VAR Hepatitis A HPV MenACWY MenB Dengue Mpox * * * See Notes RSV (Abrysvo) Seasonal administration, See Notes Recommended for all age- eligible children who lack documentation of a complete vaccination series Not recommended for all children, but is recommended for some children based on increased risk for or severe outcomes from disease Recommended for all age-eligible children, and additional doses may be necessary based on medical condition or other indications. See Notes. Precaution: Might be indicated if benefit of protection outweighs risk of adverse reaction Contraindicated or not recommended *Vaccinate after pregnancy, if indicated No Guidance/ Not Applicable a. For additional information regarding HIV laboratory parameters and use of live vaccines, see the General Best Practice Guidelines for Immunization, “Altered Immunocompetence,” at www.cdc.gov/vaccines/hcp/acip-recs/general-recs/immunocompetence.html and Table 4-1 (footnote J) at www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html. b. Severe Combined Immunodeficiency c. LAIV4 contraindicated for children 2–4 years of age with asthma or wheezing during the preceding 12 months Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 For vaccination recommendations for persons ages 19 years or older, see the Recommended Adult Immunization Schedule, 2024. Additional information y For calculating intervals between doses, 4 weeks = 28 days. Intervals of ≥4 months are determined by calendar months. y Within a number range (e.g., 12–18), a dash (–) should be read as “through.” y Vaccine doses administered ≤4 days before the minimum age or interval are considered valid. Doses of any vaccine administered ≥5 days earlier than the minimum age or minimum interval should not be counted as valid and should be repeated as age appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval. For further details, see Table 3-2, Recommended and minimum ages and intervals between vaccine doses, in General Best Practice Guidelines for Immunization at www.cdc.gov/vaccines/hcp/ acip-recs/general-recs/timing.html. y Information on travel vaccination requirements and recommendations is available at www.cdc.gov/travel/. y For vaccination of persons with immunodeficiencies, see Table 8-1, Vaccination of persons with primary and secondary immunodeficiencies, in General Best Practice Guidelines for Immunization at www.cdc.gov/vaccines/hcp/acip-recs/ general-recs/immunocompetence.html, and Immunization in Special Clinical Circumstances (In: Kimberlin DW, Barnett ED, Lynfield Ruth, Sawyer MH, eds. Red Book: 2021–2024 Report of the Committee on Infectious Diseases. 32nd ed. Itasca, IL: American Academy of Pediatrics; 2021:72–86). y For information about vaccination in the setting of a vaccine- preventable disease outbreak, contact your state or local health department. y The National Vaccine Injury Compensation Program (VICP) is a no-fault alternative to the traditional legal system for resolving vaccine injury claims. All vaccines included in the child and adolescent vaccine schedule are covered by VICP except dengue, PPSV23, RSV, Mpox and COVID-19 vaccines. Mpox and COVID-19 vaccines are covered by the Countermeasures Injury Compensation Program (CICP). For more information, see www.hrsa.gov/vaccinecompensation or www.hrsa.gov/cicp. COVID-19 vaccination (minimum age: 6 months [Moderna and Pfizer- BioNTech COVID-19 vaccines], 12 years [Novavax COVID-19 Vaccine]) Routine vaccination Age 6 months–4 years y Unvaccinated: - 2-dose series of updated (2023–2024 Formula) Moderna at 0, 4-8 weeks - 3-dose series of updated (2023–2024 Formula) Pfizer- BioNTech at 0, 3-8, 11-16 weeks y Previously vaccinated* with 1 dose of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna 4-8 weeks after the most recent dose. y Previously vaccinated* with 2 or more doses of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna at least 8 weeks after the most recent dose. y Previously vaccinated* with 1 dose of any Pfizer- BioNTech: 2-dose series of updated (2023–2024 Formula) Pfizer-BioNTech at 0, 8 weeks (minimum interval between previous Pfizer-BioNTech and dose 1: 3-8 weeks). y Previously vaccinated* with 2 or more doses of any Pfizer- BioNTech: 1 dose of updated (2023–2024 Formula) Pfizer- BioNTech at least 8 weeks after the most recent dose. Age 5–11 years y Unvaccinated: 1 dose of updated (2023–2024 Formula) Moderna or Pfizer-BioNTech vaccine. y Previously vaccinated* with 1 or more doses of Moderna or Pfizer-BioNTech: 1 dose of updated (2023–2024 Formula) Moderna or Pfizer-BioNTech at least 8 weeks after the most recent dose. Age 12–18 years y Unvaccinated: - 1 dose of updated (2023–2024 Formula) Moderna or Pfizer- BioNTech vaccine - 2-dose series of updated (2023–2024 Formula) Novavax at 0, 3-8 weeks y Previously vaccinated* with any COVID-19 vaccine(s): 1 dose of any updated (2023–2024 Formula) COVID-19 vaccine at least 8 weeks after the most recent dose. Special situations Persons who are moderately or severely immunocompromised** Age 6 months–4 years y Unvaccinated: - 3-dose series of updated (2023–2024 Formula) Moderna at 0, 4, 8 weeks - 3-dose series of updated (2023–2024 Formula) Pfizer- BioNTech at 0, 3, 11 weeks. y Previously vaccinated* with 1 dose of any Moderna: 2-dose series of updated (2023–2024 Formula) Moderna at 0, 4 weeks (minimum interval between previous Moderna and dose 1: 4 weeks). y Previously vaccinated* with 2 doses of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna at least 4 weeks after the most recent dose. y Previously vaccinated* with 3 or more doses of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna at least 8 weeks after the most recent dose. y Previously vaccinated* with 1 dose of any Pfizer- BioNTech: 2-dose series of updated (2023–2024 Formula) Pfizer-BioNTech at 0, 8 weeks (minimum interval between previous Pfizer-BioNTech and dose 1: 3 weeks). y Previously vaccinated* with 2 or more doses of any Pfizer- BioNTech: 1 dose of updated (2023–2024 Formula) Pfizer- BioNTech at least 8 weeks after the most recent dose. Age 5–11 years y Unvaccinated: - 3-dose series of updated (2023–2024 Formula) Moderna at 0, 4, 8 weeks - 3-dose series updated (2023–2024 Formula) Pfizer-BioNTech at 0, 3, 7 weeks. y Previously vaccinated* with 1 dose of any Moderna: 2-dose series of updated (2023–2024 Formula) Moderna at 0, 4 weeks (minimum interval between previous Moderna and dose 1: 4 weeks). y Previously vaccinated* with 2 doses of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna at least 4 weeks after the most recent dose. y Previously vaccinated* with 1 dose of any Pfizer- BioNTech: 2-dose series of updated (2023–2024 Formula) Pfizer-BioNTech at 0, 4 weeks (minimum interval between previous Pfizer-BioNTech and dose 1: 3 weeks) y Previously vaccinated* with 2 doses of any Pfizer- BioNTech: 1 dose of 2023–2024 Pfizer-BioNTech at least 4 weeks after the most recent dose. Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 y Previously vaccinated* with 3 or more doses of any Moderna or Pfizer-BioNTech: 1 dose of updated (2023–2024 Formula) Moderna or Pfizer-BioNTech at least 8 weeks after the most recent dose. Current COVID-19 schedule and dosage formulation available at www.cdc.gov/covidschedule. For more information on Emergency Use Authorization (EUA) indications for COVID-19 vaccines, see www.fda.gov/emergency-preparedness-and- response/coronavirus-disease-2019-covid-19/covid-19-vaccines - Prospectively: Dose 4 may be administered as early as age 12 months if at least 6 months have elapsed since dose 3. - Retrospectively: A 4th dose that was inadvertently administered as early as age 12 months may be counted if at least 4 months have elapsed since dose 3. Age 12–18 years y Unvaccinated: - 3-dose series of updated (2023–2024 Formula) Moderna at 0, 4, 8 weeks - 3-dose series of updated (2023–2024 Formula) Pfizer- BioNTech at 0, 3, 7 weeks - 2-dose series of updated (2023–2024 Formula) Novavax at 0, 3 weeks y Previously vaccinated* with 1 dose of any Moderna: 2-dose series of updated (2023–2024 Formula) Moderna at 0, 4 weeks (minimum interval between previous Moderna dose and dose 1: 4 weeks). y Previously vaccinated* with 2 doses of any Moderna: 1 dose of updated (2023–2024 Formula) Moderna at least 4 weeks after the most recent dose. y Previously vaccinated* with 1 dose of any Pfizer- BioNTech: 2-dose series of updated (2023–2024 Formula) Pfizer-BioNTech at 0, 4 weeks (minimum interval between previous Pfizer-BioNTech dose and dose 1: 3 weeks). y Previously vaccinated* with 2 doses of any Pfizer- BioNTech: 1 dose of updated (2023–2024 Formula) Pfizer- BioNTech at least 4 weeks after the most recent dose. y Previously vaccinated* with 3 or more doses of any Moderna or Pfizer-BioNTech: 1 dose of any updated (2023–2024 Formula) COVID-19 vaccine at least 8 weeks after the most recent dose. y Previously vaccinated* with 1 or more doses of Janssen or Novavax or with or without dose(s) of any Original monovalent or bivalent COVID-19 vaccine: 1 dose of any updated (2023–2024 Formula) COVID-19 vaccine at least 8 weeks after the most recent dose. There is no preferential recommendation for the use of one COVID-19 vaccine over another when more than one recommended age-appropriate vaccine is available. Administer an age-appropriate COVID-19 vaccine product for each dose. For information about transition from age 4 years to age 5 years or age 11 years to age 12 years during COVID-19 vaccination series, see Tables 1 and 2 at www.cdc.gov/vaccines/ covid-19/clinical-considerations/interim-considerations-us. html#covid-vaccines. *Note: Previously vaccinated is defined as having received any Original monovalent or bivalent COVID-19 vaccine (Janssen, Moderna, Novavax, Pfizer-BioNTech) prior to the updated 2023–2024 formulation. **Note: Persons who are moderately or severely immunocompromised have the option to receive one additional dose of updated (2023–2024 Formula) COVID-19 vaccine at least 2 months following the last recommended updated (2023 –2024 Formula) COVID-19 vaccine dose. Further additional updated (2023–2024 Formula) COVID-19 vaccine dose(s) may be administered, informed by the clinical judgement of a healthcare provider and personal preference and circumstances. Any further additional doses should be administered at least 2 months after the last updated (2023–2024 Formula) COVID-19 vaccine dose. Moderately or severely immunocompromised children 6 months–4 years of age should receive homologous updated (2023–2024 Formula) mRNA vaccine dose(s) if they receive additional doses. Dengue vaccination (minimum age: 9 years) Routine vaccination y Age 9–16 years living in areas with endemic dengue AND have laboratory confirmation of previous dengue infection - 3-dose series administered at 0, 6, and 12 months y Endemic areas include Puerto Rico, American Samoa, US Virgin Islands, Federated States of Micronesia, Republic of Marshall Islands, and the Republic of Palau. For updated guidance on dengue endemic areas and pre-vaccination laboratory testing see www.cdc.gov/mmwr/volumes/70/rr/ rr7006a1.htm?s_cid=rr7006a1_w and www.cdc.gov/dengue/ vaccine/hcp/index.html y Dengue vaccine should not be administered to children traveling to or visiting endemic dengue areas. Diphtheria, tetanus, and pertussis (DTaP) vaccination (minimum age: 6 weeks [4 years for Kinrix® or Quadracel®]) Routine vaccination y 5-dose series (3-dose primary series at age 2, 4, and 6 months, followed by a booster doses at ages 15–18 months and 4–6 years Catch-up vaccination y Dose 5 is not necessary if dose 4 was administered at age 4 years or older and at least 6 months after dose 3. y For other catch-up guidance, see Table 2. Special situations y Wound management in children less than age 7 years with history of 3 or more doses of tetanus-toxoid-containing vaccine: For all wounds except clean and minor wounds, administer DTaP if more than 5 years since last dose of tetanus-toxoid-containing vaccine. For detailed information, see www.cdc.gov/mmwr/volumes/67/rr/rr6702a1.htm. Haemophilus influenzae type b vaccination (minimum age: 6 weeks) Routine vaccination y ActHIB®, Hiberix®, Pentacel®, or Vaxelis®: 4-dose series (3-dose primary series at age 2, 4, and 6 months, followed by a booster dose* at age 12–15 months) - *Vaxelis® is not recommended for use as a booster dose. A different Hib-containing vaccine should be used for the booster dose. y PedvaxHIB®: 3-dose series (2-dose primary series at age 2 and 4 months, followed by a booster dose at age 12–15 months) Catch-up vaccination y Dose 1 at age 7–11 months: Administer dose 2 at least 4 weeks later and dose 3 (final dose) at age12–15 months or 8 weeks after dose 2 (whichever is later). y Dose 1 at age 12–14 months: Administer dose 2 (final dose) at least 8 weeks after dose 1. y Dose 1 before age 12 months and dose 2 before age 15 months: Administer dose 3 (final dose) at least 8 weeks after dose 2. y 2 doses of PedvaxHIB® before age 12 months: Administer dose 3 (final dose) at age12–59 months and at least 8 weeks after dose 2. y 1 dose administered at age 15 months or older: No further doses needed y Unvaccinated at age 15–59 months: Administer 1 dose. Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 y Previously unvaccinated children age 60 months or older who are not considered high risk: Do not require catch-up vaccination For other catch-up guidance, see Table 2. Vaxelis® can be used for catch-up vaccination in children less than age 5 years. Follow the catch-up schedule even if Vaxelis® is used for one or more doses. For detailed information on use of Vaxelis® see www.cdc.gov/mmwr/volumes/69/wr/mm6905a5.htm. Special situations y Chemotherapy or radiation treatment: Age 12–59 months - Unvaccinated or only 1 dose before age 12 months: 2 doses, 8 weeks apart - 2 or more doses before age 12 months: 1 dose at least 8 weeks after previous dose Doses administered within 14 days of starting therapy or during therapy should be repeated at least 3 months after therapy completion. y Hematopoietic stem cell transplant (HSCT): - 3-dose series 4 weeks apart starting 6 to 12 months after successful transplant, regardless of Hib vaccination history y Anatomic or functional asplenia (including sickle cell disease): Age 12–59 months - Unvaccinated or only 1 dose before age 12 months: 2 doses, 8 weeks apart - 2 or more doses before age 12 months: 1 dose at least 8 weeks after previous dose Unvaccinated* persons age 5 years or older - 1 dose y Elective splenectomy: Unvaccinated* persons age 15 months or older - 1 dose (preferably at least 14 days before procedure) y HIV infection: Age 12–59 months - Unvaccinated or only 1 dose before age 12 months: 2 doses, 8 weeks apart - 2 or more doses before age 12 months: 1 dose at least 8 weeks after previous dose Unvaccinated* persons age 5–18 years - 1 dose y Immunoglobulin deficiency, early component complement deficiency: Age 12–59 months - Unvaccinated or only 1 dose before age 12 months: 2 doses, 8 weeks apart - 2 or more doses before age 12 months: 1 dose at least 8 weeks after previous dose * Unvaccinated = Less than routine series (through age 14 months) OR no doses (age 15 months or older) Hepatitis A vaccination (minimum age: 12 months for routine vaccination) Routine vaccination y 2-dose series (minimum interval: 6 months) at age 12–23 months Catch-up vaccination y Unvaccinated persons through age 18 years should complete a 2-dose series (minimum interval: 6 months). y Persons who previously received 1 dose at age 12 months or older should receive dose 2 at least 6 months after dose 1. y Adolescents age 18 years or older may receive the combined HepA and HepB vaccine, Twinrix®, as a 3-dose series (0, 1, and 6 months) or 4-dose series (3 doses at 0, 7, and 21–30 days, followed by a booster dose at 12 months). International travel y Persons traveling to or working in countries with high or intermediate endemic hepatitis A (www.cdc.gov/travel/): - Infants age 6–11 months: 1 dose before departure; revaccinate with 2 doses (separated by at least 6 months) between age 12–23 months. - Unvaccinated age 12 months or older: Administer dose 1 as soon as travel is considered. Hepatitis B vaccination (minimum age: birth) Routine vaccination y 3-dose series at age 0, 1–2, 6–18 months (use monovalent HepB vaccine for doses administered before age 6 weeks) - Birth weight ≥2,000 grams: 1 dose within 24 hours of birth if medically stable - Birth weight <2,000 grams: 1 dose at chronological age 1 month or hospital discharge (whichever is earlier and even if weight is still <2,000 grams). y Infants who did not receive a birth dose should begin the series as soon as possible (see Table 2 for minimum intervals). y Administration of 4 doses is permitted when a combination vaccine containing HepB is used after the birth dose. y Minimum intervals (see Table 2): when 4 doses are administered, substitute “dose 4” for “dose 3” in these calculations y Final (3rd or 4th) dose: age 6–18 months (minimum age 24 weeks) y Mother is HBsAg-positive - Birth dose (monovalent HepB vaccine only): administer HepB vaccine and hepatitis B immune globulin (HBIG) (in separate limbs) within 12 hours of birth, regardless of birth weight. - Birth weight <2000 grams: administer 3 additional doses of HepB vaccine beginning at age 1 month (total of 4 doses) - Final (3rd or 4th) dose: administer at age 6 months (minimum age 24 weeks) - Test for HBsAg and anti-HBs at age 9–12 months. If HepB series is delayed, test 1–2 months after final dose. Do not test before age 9 months. y Mother is HBsAg-unknown If other evidence suggestive of maternal hepatitis B infection exists (e.g., presence of HBV DNA, HBeAg-positive, or mother known to have chronic hepatitis B infection), manage infant as if mother is HBsAg-positive - Birth dose (monovalent HepB vaccine only): Birth weight ≥2,000 grams: administer HepB vaccine within 12 hours of birth. Determine mother’s HBsAg status as soon as possible. If mother is determined to be HBsAg- positive, administer HBIG as soon as possible (in separate limb), but no later than 7 days of age. Birth weight <2,000 grams: administer HepB vaccine and HBIG (in separate limbs) within 12 hours of birth. Administer 3 additional doses of HepB vaccine beginning at age 1 month (total of 4 doses) - Final (3rd or 4th) dose: administer at age 6 months (minimum age 24 weeks) - If mother is determined to be HBsAg-positive or if status remains unknown, test for HBsAg and anti-HBs at age 9–12 months. If HepB series is delayed, test 1–2 months after final dose. Do not test before age 9 months. Catch-up vaccination y Unvaccinated persons should complete a 3-dose series at 0, 1–2, 6 months. See Table 2 for minimum intervals y Adolescents age 11–15 years may use an alternative 2-dose schedule with at least 4 months between doses (adult formulation Recombivax HB® only). y Adolescents age 18 years may receive: - Heplisav-B®: 2-dose series at least 4 weeks apart - PreHevbrio®: 3-dose series at 0, 1, and 6 months - Combined HepA and HepB vaccine, Twinrix®: 3-dose series (0, 1, and 6 months) or 4-dose series (3 doses at 0, 7, and 21–30 days, followed by a booster dose at 12 months). Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Special situations y Revaccination is not generally recommended for persons with a normal immune status who were vaccinated as infants, children, adolescents, or adults. y Post-vaccination serology testing and revaccination (if anti-HBs <10mlU/mL) is recommended for certain populations, including: - Infants born to HBsAg-positive mothers - Persons who are predialysis or on maintenance dialysis - Other immunocompromised persons - For detailed revaccination recommendations, see www.cdc. gov/vaccines/hcp/acip-recs/vacc-specific/hepb.html. Note: Heplisav-B and PreHevbrio are not recommended in pregnancy due to lack of safety data in pregnant persons Human papillomavirus vaccination (minimum age: 9 years) Routine and catch-up vaccination y HPV vaccination routinely recommended at age 11–12 years (can start at age 9 years) and catch-up HPV vaccination recommended for all persons through age 18 years if not adequately vaccinated y 2- or 3-dose series depending on age at initial vaccination: - Age 9–14 years at initial vaccination: 2-dose series at 0, 6–12 months (minimum interval: 5 months; repeat dose if administered too soon) - Age 15 years or older at initial vaccination: 3-dose series at 0, 1–2 months, 6 months (minimum intervals: dose 1 to dose 2: 4 weeks / dose 2 to dose 3: 12 weeks / dose 1 to dose 3: 5 months; repeat dose if administered too soon) y No additional dose recommended when any HPV vaccine series of any valency has been completed using recommended dosing intervals. Special situations y Immunocompromising conditions, including HIV infection: 3-dose series, even for those who initiate vaccination at age 9 through 14 years. y History of sexual abuse or assault: Start at age 9 years y Pregnancy: Pregnancy testing not needed before vaccination; HPV vaccination not recommended until after pregnancy; no intervention needed if vaccinated while pregnant Influenza vaccination (minimum age: 6 months [IIV], 2 years [LAIV4], 18 years [recombinant influenza vaccine, RIV4]) Special situations y International travel Routine vaccination y Use any influenza vaccine appropriate for age and health status annually: - Age 6 months–8 years who have received fewer than 2 influenza vaccine doses before July 1, 2023, or whose influenza vaccination history is unknown: 2 doses, separated by at least 4 weeks. Administer dose 2 even if the child turns 9 years between receipt of dose 1 and dose 2. - Age 6 months–8 years who have received at least 2 influenza vaccine doses before July 1, 2023: 1 dose - Age 9 years or older: 1 dose y For the 2023-2024 season, see www.cdc.gov/mmwr/ volumes/72/rr/rr7202a1.htm. y For the 2024–25 season, see the 2024–25 ACIP influenza vaccine recommendations. Special situations y Close contacts (e.g., household contacts) of severely immunosuppressed persons who require a protected environment: should not receive LAIV4. If LAIV4 is given, they should avoid contact with for such immunosuppressed persons for 7 days after vaccination. Note: Persons with an egg allergy can receive any influenza vaccine (egg-based and non-egg-based) appropriate for age and health status. Measles, mumps, and rubella vaccination (minimum age: 12 months for routine vaccination) Routine vaccination y 2-dose series at age 12–15 months, age 4–6 years y MMR or MMRV* may be administered Note: For dose 1 in children age 12–47 months, it is recommended to administer MMR and varicella vaccines separately. MMRV* may be used if parents or caregivers express a preference. Catch-up vaccination y Unvaccinated children and adolescents: 2-dose series at least 4 weeks apart* y The maximum age for use of MMRV* is 12 years. - Infants age 6–11 months: 1 dose before departure; revaccinate with 2-dose series at age 12–15 months (12 months for children in high-risk areas) and dose 2 as early as 4 weeks later.* - Unvaccinated children age 12 months or older: 2-dose series at least 4 weeks apart before departure* y In mumps outbreak settings, for information about additional doses of MMR (including 3rd dose of MMR), see www.cdc.gov/mmwr/volumes/67/wr/mm6701a7.htm *Note: If MMRV is used, the minimum interval between MMRV doses is 3 months Meningococcal serogroup A,C,W,Y vaccination (minimum age: 2 months [MenACWY-CRM, Menveo], 2 years [MenACWY-TT, MenQuadfi]), 10 years [MenACWY-TT/MenB-FHbp, Penbraya]) Routine vaccination y 2-dose series at age 11–12 years; 16 years Catch-up vaccination y Age 13–15 years: 1 dose now and booster at age 16–18 years (minimum interval: 8 weeks) y Age 16–18 years: 1 dose Special situations Anatomic or functional asplenia (including sickle cell disease), HIV infection, persistent complement component deficiency, complement inhibitor (e.g., eculizumab, ravulizumab) use: y Menveo®* - Dose 1 at age 2 months: 4-dose series (additional 3 doses at age 4, 6, and 12 months) - Dose 1 at age 3–6 months: 3- or 4-dose series (dose 2 [and dose 3 if applicable] at least 8 weeks after previous dose until a dose is received at age 7 months or older, followed by an additional dose at least 12 weeks later and after age 12 months) - Dose 1 at age 7–23 months: 2-dose series (dose 2 at least 12 weeks after dose 1 and after age 12 months) - Dose 1 at age 24 months or older: 2-dose series at least 8 weeks apart y MenQuadfi® - Dose 1 at age 24 months or older: 2-dose series at least 8 weeks apart Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Travel to countries with hyperendemic or epidemic meningococcal disease, including countries in the African meningitis belt or during the Hajj (www.cdc.gov/travel/): y Children less than age 24 months: - Menveo®* (age 2–23 months) Dose 1 at age 2 months: 4-dose series (additional 3 doses at age 4, 6, and 12 months) Dose 1 at age 3–6 months: 3- or 4-dose series (dose 2 [and dose 3 if applicable] at least 8 weeks after previous dose until a dose is received at age 7 months or older, followed by an additional dose at least 12 weeks later and after age 12 months) Dose 1 at age 7–23 months: 2-dose series (dose 2 at least 12 weeks after dose 1 and after age 12 months) y Children age 2 years or older: 1 dose Menveo®* or MenQuadfi® First-year college students who live in residential housing (if not previously vaccinated at age 16 years or older) or military recruits: y 1 dose Menveo®* or MenQuadfi® Adolescent vaccination of children who received MenACWY prior to age 10 years: y Children for whom boosters are recommended because of an ongoing increased risk of meningococcal disease (e.g., those with complement component deficiency, HIV, or asplenia): Follow the booster schedule for persons at increased risk. y Children for whom boosters are not recommended (e.g., a healthy child who received a single dose for travel to a country where meningococcal disease is endemic): Administer MenACWY according to the recommended adolescent schedule with dose 1 at age 11–12 years and dose 2 at age 16 years. * Menveo has two formulations: lyophilized and liquid. The liquid formulation should not be used before age 10 years. See www. cdc.gov/vaccines/vpd/mening/downloads/menveo-single-vial- presentation.pdf. Note: For MenACWY booster dose recommendations for groups listed under “Special situations” and in an outbreak setting and additional meningococcal vaccination information, see www.cdc.gov/mmwr/volumes/69/rr/rr6909a1.htm. Children age 10 years or older may receive a single dose of Penbraya™ as an alternative to separate administration of MenACWY and MenB when both vaccines would be given on the same clinic day (see “Meningococcal serogroup B vaccination” section below for more information). Meningococcal serogroup B vaccination (minimum age: 10 years [MenB-4C, Bexsero®; MenB-FHbp, Trumenba®; MenACWY-TT/MenB-FHbp, Penbraya™]) Shared clinical decision-making y Adolescents not at increased risk age 16–23 years (preferred age 16–18 years) based on shared clinical decision-making: - Bexsero®: 2-dose series at least 1 month apart - Trumenba®: 2-dose series at least 6 months apart (if dose 2 is administered earlier than 6 months, administer a 3rd dose at least 4 months after dose 2) For additional information on shared clinical decision-making for MenB, see www.cdc.gov/vaccines/hcp/admin/downloads/ isd-job-aid-scdm-mening-b-shared-clinical-decision-making.pdf Special situations Anatomic or functional asplenia (including sickle cell disease), persistent complement component deficiency, complement inhibitor (e.g., eculizumab, ravulizumab) use: y Bexsero®: 2-dose series at least 1 month apart y Trumenba®: 3-dose series at 0, 1–2, 6 months (if dose 2 was administered at least 6 months after dose 1, dose 3 not needed; if dose 3 is administered earlier than 4 months after dose 2, a 4th dose should be administered at least 4 months after dose 3) Note: Bexsero® and Trumenba® are not interchangeable; the same product should be used for all doses in a series. For MenB booster dose recommendations for groups listed under “Special situations” and in an outbreak setting and additional meningococcal vaccination information, see www.cdc.gov/mmwr/volumes/69/rr/rr6909a1.htm. Children age 10 years or older may receive a dose of Penbraya™ as an alternative to separate administration of MenACWY and MenB when both vaccines would be given on the same clinic day. For age-eligible children not at increased risk, if Penbraya™ is used for dose 1 MenB, MenB-FHbp (Trumenba) should be administered for dose 2 MenB. For age-eligible children at increased risk of meningococcal disease, Penbraya™ may be used for additional MenACWY and MenB doses (including booster doses) if both would be given on the same clinic day and at least 6 months have elapsed since most recent Penbraya™ dose. Mpox vaccination (minimum age: 18 years [Jynneos®]) Special situations y Age 18 years and at risk for Mpox infection: 2-dose series, 28 days apart. Risk factors for Mpox infection include: - Persons who are gay, bisexual, and other MSM, transgender or nonbinary people who in the past 6 months have had: A new diagnosis of at least 1 sexually transmitted disease More than 1 sex partner Sex at a commercial sex venue Sex in association with a large public event in a geographic area where Mpox transmission is occurring - Persons who are sexual partners of the persons described above - Persons who anticipate experiencing any of the situations described above y Pregnancy: There is currently no ACIP recommendation for Jynneos use in pregnancy due to lack of safety data in pregnant persons. Pregnant persons with any risk factor described above may receive Jynneos. For detailed information, see: www.cdc.gov/vaccines/acip/ meetings/downloads/slides-2023-10-25-26/04-MPOX-Rao-508.pdf Pneumococcal vaccination (minimum age: 6 weeks [PCV15], [PCV 20]; 2 years [PPSV23]) Routine vaccination with PCV y 4-dose series at 2, 4, 6, 12–15 months Catch-up vaccination with PCV y Healthy children ages 2–4 years with any incomplete* PCV series: 1 dose PCV y For other catch-up guidance, see Table 2. Note: For children without risk conditions, PCV20 is not indicated if they have received 4 doses of PCV13 or PCV15 or another age appropriate complete PCV series. Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Age 2–5 years y Any incomplete* PCV series: Poliovirus vaccination (minimum age: 6 weeks) y Completed recommended PCV series but have not received Age 6–18 years Special situations Children and adolescents with cerebrospinal fluid leak; chronic heart disease; chronic kidney disease (excluding maintenance dialysis and nephrotic syndrome); chronic liver disease; chronic lung disease (including moderate persistent or severe persistent asthma); cochlear implant; or diabetes mellitus: Age 2–5 years y Any incomplete* PCV series with: - 3 PCV doses: 1 dose PCV (at least 8 weeks after the most recent PCV dose) - Less than 3 PCV doses: 2 doses PCV (at least 8 weeks after the most recent dose and administered at least 8 weeks apart) PPSV23 - Previously received at least 1 dose of PCV20: no further PCV or PPSV23 doses needed - Not previously received PCV20: administer 1 dose PCV20 OR 1 dose PPSV23 administer at least 8 weeks after the most recent PCV dose. Age 6–18 years y Not previously received any dose of PCV13, PCV15, or PCV20: administer 1 dose of PCV15 or PCV20. If PCV15 is used and no previous receipt of PPSV23, administer 1 dose of PPSV23 at least 8 weeks after the PCV15 dose.** y Received PCV before age 6 years but have not received PPSV23 - Previously received at least 1 dose of PCV20: no further PCV or PPSV23 doses needed - Not previously received PCV20: 1 dose PCV20 OR 1 dose PPSV23 administer at least 8 weeks after the most recent PCV dose. y Received PCV13 only at or after age 6 years: administer 1 dose PCV20 OR 1 dose PPSV23 at least 8 weeks after the most recent PCV13 dose. y Received 1 dose PCV13 and 1 dose PPSV23 at or after age 6 years: no further doses of any PCV or PPSV23 indicated. Children and adolescents on maintenance dialysis, or with immunocompromising conditions such as nephrotic syndrome; congenital or acquired asplenia or splenic dysfunction; congenital or acquired immunodeficiencies; diseases and conditions treated with immunosuppressive drugs or radiation therapy, including malignant neoplasms, leukemias, lymphomas, Hodgkin disease, and solid organ transplant; HIV infection; or sickle cell disease or other hemoglobinopathies: - 3 PCV doses: 1 dose PCV (at least 8 weeks after the most recent PCV dose) - Less than 3 PCV doses: 2 doses PCV (at least 8 weeks after the most recent dose and administered at least 8 weeks apart) y Completed recommended PCV series but have not received PPSV23 - Previously received at least 1 dose of PCV20: no further PCV or PPSV23 doses needed - Not previously received PCV20: administer 1 dose PCV20 OR 1 dose PPSV23 at least 8 weeks after the most recent PCV dose. If PPSV23 is used, administer 1 dose of PCV20 or dose 2 PPSV23 at least 5 years after dose 1 PPSV23. y Not previously received any dose of PCV13, PCV15, or PCV20: administer 1 dose of PCV15 or 1 dose of PCV20. If PCV15 is used and no previous receipt of PPSV23, administer 1 dose of PPSV23 at least 8 weeks after the PCV15 dose.** y Received PCV before age 6 years but have not received PPSV23 - Previously received at least 1 dose of PCV20: no additional dose of PCV or PPSV23 - Not previously received PCV20: administer 1 dose PCV20 OR 1 dose PPSV23 at least 8 weeks after the most recent PCV dose. If PPSV23 is used, administer either PCV20 or dose 2 PPSV23 at least 5 years after dose 1 PPSV23. y Received PCV13 only at or after age 6 years: administer 1 dose PCV20 OR 1 dose PPSV23 at least 8 weeks after the most recent PCV13 dose. If PPSV23 is used, administer 1 dose of PCV20 or dose 2 PPSV23 at least 5 years after dose 1 PPSV23. y Received 1 dose PCV13 and 1 dose PPSV23 at or after age 6 years: administer 1 dose PCV20 OR 1 dose PPSV23 at least 8 weeks after the most recent PCV13 dose and at least 5 years after dose 1 PPSV23. *Incomplete series = Not having received all doses in either the recommended series or an age-appropriate catch-up series. See Table 2 in ACIP pneumococcal recommendations at stacks.cdc.gov/view/cdc/133252 **When both PCV15 and PPSV23 are indicated, administer all doses of PCV15 first. PCV15 and PPSV23 should not be administered during the same visit. For guidance on determining which pneumococcal vaccines a patient needs and when, please refer to the mobile app, which can be downloaded here: www.cdc.gov/vaccines/vpd/ pneumo/hcp/pneumoapp.html Routine vaccination y 4-dose series at ages 2, 4, 6–18 months, 4–6 years; administer the final dose on or after age 4 years and at least 6 months after the previous dose. y 4 or more doses of IPV can be administered before age 4 years when a combination vaccine containing IPV is used. However, a dose is still recommended on or after age 4 years and at least 6 months after the previous dose. Catch-up vaccination y In the first 6 months of life, use minimum ages and intervals only for travel to a polio-endemic region or during an outbreak. y Adolescents age 18 years known or suspected to be unvaccinated or incompletely vaccinated: administer remaining doses (1, 2, or 3 IPV doses) to complete a 3-dose primary series.* Unless there are specific reasons to believe they were not vaccinated, most persons aged 18 years or older born and raised in the United States can assume they were vaccinated against polio as children. Series containing oral poliovirus vaccine (OPV), either mixed OPV-IPV or OPV-only series: y Total number of doses needed to complete the series is the same as that recommended for the U.S. IPV schedule. See www.cdc.gov/mmwr/volumes/66/wr/mm6601a6.htm?s_%20 cid=mm6601a6_w. y Only trivalent OPV (tOPV) counts toward the U.S. vaccination requirements. - Doses of OPV administered before April 1, 2016, should be counted (unless specifically noted as administered during a campaign). - Doses of OPV administered on or after April 1, 2016, should not be counted. - For guidance to assess doses documented as “OPV,” see www.cdc.gov/mmwr/volumes/66/wr/mm6606a7.htm?s_ cid=mm6606a7_w. y For other catch-up guidance, see Table 2. Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Special situations y Adolescents aged 18 years at increased risk of exposure to poliovirus and completed primary series*: may administer one lifetime IPV booster *Note: Complete primary series consist of at least 3 doses of IPV or trivalent oral poliovirus vaccine (tOPV) in any combination. For detailed information, see: www.cdc.gov/vaccines/vpd/ polio/hcp/recommendations.html Respiratory syncytial virus immunization (minimum age: birth [Nirsevimab, RSV-mAb (Beyfortus™) Routine immunization y Infants born October – March in most of the continental United States* - Mother did not receive RSV vaccine OR mother’s RSV vaccination status is unknown: administer 1 dose nirsevimab within 1 week of birth in hospital or outpatient setting - Mother received RSV vaccine less than 14 days prior to delivery: administer 1 dose nirsevimab within 1 week of birth in hospital or outpatient setting - Mother received RSV vaccine at least 14 days prior to delivery: nirsevimab not needed but can be considered in rare circumstances at the discretion of healthcare providers (see special populations and situations at www.cdc.gov/vaccines/vpd/rsv/hcp/child-faqs.html) y Infants born April–September in most of the continental United States* - Mother did not receive RSV vaccine OR mother’s RSV vaccination status is unknown: administer 1 dose nirsevimab shortly before start of RSV season* - Mother received RSV vaccine less than 14 days prior to delivery: administer 1 dose nirsevimab shortly before start of RSV season* - Mother received RSV vaccine at least 14 days prior to delivery: nirsevimab not needed but can be considered in rare circumstances at the discretion of healthcare providers(see special populations and situations at www.cdc.gov/vaccines/vpd/rsv/hcp/child-faqs.html) Infants with prolonged birth hospitalization** (e.g., for prematurity) discharged October through March should be immunized shortly before or promptly after discharge. Special situations y Ages 8–19 months with chronic lung disease of prematurity requiring medical support (e.g., chronic corticosteroid therapy, diuretic therapy, or supplemental oxygen) any time during the 6-month period before the start of the second RSV season; severe immunocompromise; cystic fibrosis with either weight for length <10th percentile or manifestation of severe lung disease (e.g., previous hospitalization for pulmonary exacerbation in the first year of life or abnormalities on chest imaging that persist when stable)**: - 1 dose nirsevimab shortly before start of second RSV season* y Ages 8–19 months who are American Indian or Alaska Native: - 1 dose nirsevimab shortly before start of second RSV season* y Age-eligible and undergoing cardiac surgery with cardiopulmonary bypass**: 1 additional dose of nirsevimab after surgery. For additional details see special populations and situations at www.cdc.gov/vaccines/vpd/rsv/hcp/child- faqs.html *Note: While the timing of the onset and duration of RSV season may vary, nirsevimab may be administered October through March in most of the continental United States. Providers in jurisdictions with RSV seasonality that differs from most of the continental United States (e.g., Alaska, jurisdiction with tropical climate) should follow guidance from public health authorities (e.g., CDC, health departments) or regional medical centers on timing of administration based on local RSV seasonality. Although optimal timing of administration is just before the start of the RSV season, nirsevimab may also be administered during the RSV season to infants and children who are age-eligible. **Note: Nirsevimab can be administered to children who are eligible to receive palivizumab. Children who have received nirsevimab should not receive palivizumab for the same RSV season. For further guidance, see www.cdc.gov/mmwr/volumes/72/ wr/mm7234a4.htm and www.cdc.gov/vaccines/vpd/rsv/hcp/ child-faqs.html Respiratory syncytial virus vaccination (RSV [Abrysvo™]) Routine vaccination y Pregnant at 32 weeks 0 days through 36 weeks and 6 days gestation from September through January in most of the continental United States*: 1 dose RSV vaccine (Abrysvo™). Administer RSV vaccine regardless of previous RSV infection. - Either maternal RSV vaccination or infant immunization with nirsevimab (RSV monoclonal antibody) is recommended to prevent respiratory syncytial virus lower respiratory tract infection in infants. y All other pregnant persons: RSV vaccine not recommended. There is currently no ACIP recommendation for RSV vaccination in subsequent pregnancies. No data are available to inform whether additional doses are needed in later pregnancies. *Note: Providers in jurisdictions with RSV seasonality that differs from most of the continental United States (e.g., Alaska, jurisdiction with tropical climate) should follow guidance from public health authorities (e.g., CDC, health departments) or regional medical centers on timing of administration based on local RSV seasonality. Rotavirus vaccination (minimum age: 6 weeks) Routine vaccination y Rotarix®: 2-dose series at age 2 and 4 months y RotaTeq®: 3-dose series at age 2, 4, and 6 months y If any dose in the series is either RotaTeq® or unknown, default to 3-dose series. Catch-up vaccination y Do not start the series on or after age 15 weeks, 0 days. y The maximum age for the final dose is 8 months, 0 days. y For other catch-up guidance, see Table 2. Notes Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Varicella vaccination (minimum age: 12 months) Routine vaccination y 2-dose series at age 12–15 months, 4–6 years y VAR or MMRV may be administered* y Dose 2 may be administered as early as 3 months after dose 1 (a dose inadvertently administered after at least 4 weeks may be counted as valid) *Note: For dose 1 in children age 12–47 months, it is recommended to administer MMR and varicella vaccines separately. MMRV may be used if parents or caregivers express a preference. Catch-up vaccination y Ensure persons age 7–18 years without evidence of immunity (see MMWR at www.cdc.gov/mmwr/pdf/rr/rr5604.pdf ) have a 2-dose series: - Age 7–12 years: Routine interval: 3 months (a dose inadvertently administered after at least 4 weeks may be counted as valid) - Age 13 years and older: Routine interval: 4–8 weeks (minimum interval: 4 weeks) - The maximum age for use of MMRV is 12 years. Tetanus, diphtheria, and pertussis (Tdap) vaccination (minimum age: 11 years for routine vaccination, 7 years for catch-up vaccination) Routine vaccination y Age 11–12 years: 1 dose Tdap (adolescent booster) y Pregnancy: 1 dose Tdap during each pregnancy, preferably in early part of gestational weeks 27–36. Note: Tdap may be administered regardless of the interval since the last tetanus- and diphtheria-toxoid-containing vaccine. Catch-up vaccination y Age 13–18 years who have not received Tdap: 1 dose Tdap (adolescent booster) y Age 7–18 years not fully vaccinated* with DTaP: 1 dose Tdap as part of the catch-up series (preferably the first dose); if additional doses are needed, use Td or Tdap. y Tdap administered at age 7–10 years: - Age 7–9 years who receive Tdap should receive the adolescent Tdap booster dose at age 11–12 years. - Age 10 years who receive Tdap do not need the adolescent Tdap booster dose at age 11–12 years. y DTaP inadvertently administered on or after age 7 years: - Age 7–9 years: DTaP may count as part of catch-up series. Administer adolescent Tdap booster dose at age 11–12 years. - Age 10–18 years: Count dose of DTaP as the adolescent Tdap booster dose. y For other catch-up guidance, see Table 2. Special situations y Wound management in persons age 7 years or older with history of 3 or more doses of tetanus-toxoid-containing vaccine: For clean and minor wounds, administer Tdap or Td if more than 10 years since last dose of tetanus-toxoid- containing vaccine; for all other wounds, administer Tdap or Td if more than 5 years since last dose of tetanus-toxoid- containing vaccine. Tdap is preferred for persons age 11 years or older who have not previously received Tdap or whose Tdap history is unknown. If a tetanus-toxoid-containing vaccine is indicated for a pregnant adolescent, use Tdap. y For detailed information, see www.cdc.gov/mmwr/ volumes/69/wr/mm6903a5.htm. *Fully vaccinated = 5 valid doses of DTaP OR 4 valid doses of DTaP if dose 4 was administered at age 4 years or older 11/16/2023 Centers for Disease Control and Prevention | Recommended Child and Adolescent Immunization Schedule, United States, 2024 COVID-19 protein subunit vaccine [Novavax] • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a component of a Novavax COVID-19 vaccine4 Appendix Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Guide to Contraindications and Precautions to Commonly Used Vaccines Adapted from Table 4-1 in Advisory Committee on Immunization Practices (ACIP) General Best Practice Guidelines for Immunization: Contraindication and Precautions, Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2023–24 Influenza Season | MMWR (cdc.gov), Contraindications and Precautions for COVID-19 Vaccination, and Contraindications and Precautions for JYNNEOS Vaccination Vaccines and other Immunizing Agents COVID-19 mRNA vaccines [Pfizer-BioNTech, Moderna] Contraindicated or Not Recommended1 Precautions2 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a component of an mRNA COVID-19 vaccine4 • Diagnosed non-severe allergy (e.g., urticaria beyond the injection site) to a component of an mRNA COVID-19 vaccine4; or non-severe, immediate (onset less than 4 hours) allergic reaction after administration of a previous dose of an mRNA COVID-19 vaccine • Myocarditis or pericarditis within 3 weeks after a dose of any COVID-19 vaccine • Multisystem inflammatory syndrome in children (MIS-C) or multisystem inflammatory syndrome in adults (MIS-A) • Moderate or severe acute illness, with or without fever • Diagnosed non-severe allergy (e.g., urticaria beyond the injection site) to a component of Novavax COVID-19 vaccine4; or non-severe, immediate (onset less than 4 hours) allergic reaction after administration of a previous dose of a Novavax COVID-19 vaccine • Myocarditis or pericarditis within 3 weeks after a dose of any COVID-19 vaccine • Multisystem inflammatory syndrome in children (MIS-C) or multisystem inflammatory syndrome in adults (MIS-A) • Moderate or severe acute illness, with or without fever type of influenza vaccine • Persons with a history of severe allergic reaction (e.g., anaphylaxis) after a previous dose of any egg-based IIV, RIV, or LAIV of any valency. If using ccIV4, administer in medical setting under supervision of health care provider who can recognize and manage severe allergic reactions. May consult an allergist. • Moderate or severe acute illness with or without fever type of influenza vaccine • Persons with a history of severe allergic reaction (e.g., anaphylaxis) after a previous dose of any egg-based IIV, ccIIV, or LAIV of any valency. If using RIV4, administer in medical setting under supervision of health care provider who can recognize and manage severe allergic reactions. May consult an allergist. • Moderate or severe acute illness with or without fever • Asthma in persons age 5 years old or older • Persons with underlying medical conditions other than those listed under contraindications that might predispose to complications after wild-type influenza virus infection, e.g., chronic pulmonary, cardiovascular (except isolated hypertension), renal, hepatic, neurologic, hematologic, or metabolic disorders (including diabetes mellitus) • Moderate or severe acute illness with or without fever • Severe allergic reaction (e.g., anaphylaxis) after previous dose of any influenza vaccine • Guillain-Barré syndrome (GBS) within 6 weeks after a previous dose of any (i.e., any egg-based IIV, ccIIV, RIV, or LAIV of any valency) type of influenza vaccine • Severe allergic reaction (e.g., anaphylaxis) to any vaccine component3 (excluding egg) • Moderate or severe acute illness with or without fever • Severe allergic reaction (e.g., anaphylaxis) to any ccIIV of any valency, or to any component3 of ccIIV4 • Guillain-Barré syndrome (GBS) within 6 weeks after a previous dose of any • Severe allergic reaction (e.g., anaphylaxis) to any RIV of any valency, or to any component3 of RIV4 • Guillain-Barré syndrome (GBS) within 6 weeks after a previous dose of any Influenza, egg-based, inactivated injectable (IIV4) Influenza, cell culture-based inactivated injectable (ccIIV4) [Flucelvax Quadrivalent] Influenza, recombinant injectable (RIV4) [Flublok Quadrivalent] Influenza, live attenuated (LAIV4) [Flumist Quadrivalent] • Severe allergic reaction (e.g., anaphylaxis) after previous dose of any influenza vaccine • Guillain-Barré syndrome (GBS) within 6 weeks after a previous dose of any (i.e., any egg-based IIV, ccIIV, RIV, or LAIV of any valency) type of influenza vaccine • Severe allergic reaction (e.g., anaphylaxis) to any vaccine component3 (excluding egg) • Children age 2–4 years with a history of asthma or wheezing • Anatomic or functional asplenia • Immunocompromised due to any cause including, but not limited to, medications and HIV infection • Close contacts or caregivers of severely immunosuppressed persons who require a protected environment • Pregnancy • Cochlear implant • Active communication between the cerebrospinal fluid (CSF) and the oropharynx, nasopharynx, nose, ear or any other cranial CSF leak • Children and adolescents receiving aspirin or salicylate-containing medications • Received influenza antiviral medications oseltamivir or zanamivir within the previous 48 hours, peramivir within the previous 5 days, or baloxavir within the previous 17 days 1. When a contraindication is present, a vaccine should NOT be administered. Kroger A, Bahta L, Hunter P. ACIP General Best Practice Guidelines for Immunization. 2. When a precaution is present, vaccination should generally be deferred but might be indicated if the benefit of protection from the vaccine outweighs the risk for an adverse reaction. Kroger A, Bahta L, Hunter P. ACIP General Best Practice Guidelines for Immunization. 3. Vaccination providers should check FDA-approved prescribing information for the most complete and updated information, including contraindications, warnings, and precautions. See Package inserts for U.S.-licensed vaccines. 4. See package inserts and FDA EUA fact sheets for a full list of vaccine ingredients. mRNA COVID-19 vaccines contain polyethylene glycol (PEG). Haemophilus influenzae type b (Hib) Hepatitis A (HepA) Hepatitis B (HepB) • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Less than age 6 weeks • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 including neomycin • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 including yeast • Pregnancy: Heplisav-B and PreHevbrio are not recommended due to lack of safety data in pregnant persons. Use other hepatitis B vaccines if HepB is indicated4. Hepatitis A-Hepatitis B vaccine (HepA-HepB) [Twinrix] yeast Human papillomavirus (HPV) Appendix Vaccines and other Immunizing Agents Dengue (DEN4CYD) Diphtheria, tetanus, pertussis (DTaP) Measles, mumps, rubella (MMR) Measles, mumps, rubella, and varicella (MMRV) Meningococcal ACWY (MenACWY) MenACWY-CRM [Menveo] MenACWY-TT [MenQuadfi] Meningococcal B (MenB) MenB-4C [Bexsero] MenB-FHbp [Trumenba] Meningococcal ABCWY (MenACWY-TT/MenB-FHbp) [Penbraya] Mpox [Jynneos] Pneumococcal conjugate (PCV) Pneumococcal polysaccharide (PPSV23) Poliovirus vaccine, inactivated (IPV) RSV monoclonal antibody (RSV-mAb) Respiratory syncytial virus vaccine (RSV) Rotavirus (RV) RV1 [Rotarix] RV5 [RotaTeq] Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 Contraindicated or Not Recommended1 Precautions2 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe immunodeficiency (e.g., hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, long-term immunosuppressive therapy or patients with HIV infection who are severely immunocompromised) • Lack of laboratory confirmation of a previous Dengue infection • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • For DTaP only: Encephalopathy (e.g., coma, decreased level of consciousness, prolonged seizures) not attributable to another identifiable cause within 7 days of administration of previous dose of DTP or DTaP • Pregnancy • HIV infection without evidence of severe immunosuppression • Moderate or severe acute illness with or without fever • Guillain-Barré syndrome (GBS) within 6 weeks after previous dose of tetanus-toxoid–containing vaccine • History of Arthus-type hypersensitivity reactions after a previous dose of diphtheria-toxoid–containing or tetanus-toxoid–containing vaccine; defer vaccination until at least 10 years have elapsed since the last tetanus-toxoid-containing vaccine • For DTaP only: Progressive neurologic disorder, including infantile spasms, uncontrolled epilepsy, progressive encephalopathy; defer DTaP until neurologic status clarified and stabilized • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 including neomycin and • Moderate or severe acute illness with or without fever • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Pregnancy: HPV vaccination not recommended. • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe immunodeficiency (e.g., hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, long-term immunosuppressive therapy or patients with HIV infection who are severely immunocompromised) • Pregnancy • Family history of altered immunocompetence, unless verified clinically or by laboratory testing as immunocompetent • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • For Men ACWY-CRM only: severe allergic reaction to any diphtheria toxoid—or CRM197—containing vaccine • For MenACWY-TT only: severe allergic reaction to a tetanus toxoid-containing vaccine • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Moderate or severe acute illness with or without fever • Recent (≤11 months) receipt of antibody-containing blood product (specific interval depends on product) • History of thrombocytopenia or thrombocytopenic purpura • Need for tuberculin skin testing or interferon-gamma release assay (IGRA) testing • Moderate or severe acute illness with or without fever • For MMRV only: Personal or family (i.e., sibling or parent) history of seizures of any etiology • For MenACWY-CRM only: Preterm birth if less than age 9 months • Moderate or severe acute illness with or without fever • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction to a tetanus toxoid-containing vaccine • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction (e.g., anaphylaxis) to any diphtheria-toxoid-containing vaccine or its component3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component5 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe combined immunodeficiency (SCID) • History of intussusception • Pregnancy • For MenB-4C only: Latex sensitivity • Moderate or severe acute illness with or without fever • Moderate or severe acute illness, with or without fever • Moderate or severe acute illness, with or without fever • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Pregnancy • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Moderate or severe acute illness with or without fever • Altered immunocompetence other than SCID • Chronic gastrointestinal disease • RV1 only: Spina bifida or bladder exstrophy • Moderate or severe acute illness with or without fever Tetanus, diphtheria, and acellular pertussis (Tdap) Tetanus, diphtheria (Td) • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • For Tdap only: Encephalopathy (e.g., coma, decreased level of consciousness, prolonged seizures) not attributable to another identifiable cause within 7 days of administration of previous dose of DTP, DTaP, or Tdap Varicella (VAR) • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component3 • Severe immunodeficiency (e.g., hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, long-term immunosuppressive therapy or patients with HIV infection who are severely immunocompromised) • Pregnancy • Family history of altered immunocompetence, unless verified clinically or by laboratory testing as immunocompetent • Guillain-Barré syndrome (GBS) within 6 weeks after a previous dose of tetanus-toxoid–containing vaccine • History of Arthus-type hypersensitivity reactions after a previous dose of diphtheria-toxoid–containing or tetanus-toxoid–containing vaccine; defer vaccination until at least 10 years have elapsed since the last tetanus-toxoid–containing vaccine • For Tdap only: Progressive or unstable neurological disorder, uncontrolled seizures, or progressive encephalopathy until a treatment regimen has been established and the condition has stabilized • Moderate or severe acute illness with or without fever • Recent (≤11 months) receipt of antibody-containing blood product (specific interval depends on product) • Receipt of specific antiviral drugs (acyclovir, famciclovir, or valacyclovir) 24 hours before vaccination (avoid use of these antiviral drugs for 14 days after vaccination) • Use of aspirin or aspirin-containing products • Moderate or severe acute illness with or without fever • If using MMRV, see MMR/MMRV for additional precautions 1. When a contraindication is present, a vaccine should NOT be administered. Kroger A, Bahta L, Hunter P. ACIP General Best Practice Guidelines for Immunization. www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html 2. When a precaution is present, vaccination should generally be deferred but might be indicated if the benefit of protection from the vaccine outweighs the risk for an adverse reaction. Kroger A, Bahta L, Hunter P. ACIP General Best Practice Guidelines for 3. Vaccination providers should check FDA-approved prescribing information for the most complete and updated information, including contraindications, warnings, and precautions. Package inserts for U.S.-licensed vaccines are available at Immunization. www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html www.fda.gov/vaccines-blood-biologics/approved-products/vaccines-licensed-use-united-states. 4. For information on the pregnancy exposure registries for persons who were inadvertently vaccinated with Heplisav-B or PreHevbrio while pregnant, please visit heplisavbpregnancyregistry.com or www.prehevbrio.com/#safety. 5. Full prescribing information for BEYFORTUS (nirsevimab-alip) www.accessdata.fda.gov/drugsatfda_docs/label/2023/761328s000lbl.pdf Addendum Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States, 2024 In addition to the recommendations presented in the previous sections of this immunization schedule, ACIP has approved the following recommendations by majority vote since October 26, 2023. The following recommendations have been adopted by the CDC Director and are now official. Links are provided if these recommendations have been published in Morbidity and Mortality Weekly Report (MMWR). Vaccines Recommendations COVID-19 (Moderna, Pfizer-BioNTech, Novavax) • ACIP recommends 2024-2025 COVID-19 vaccines as authorized or approved by FDA in persons ≥6 months of age. June 27, 2024 Effective Date of Recommendation* Influenza • ACIP reaffirms the recommendation for routine annual influenza vaccination of all persons aged ≥6 months who do not June 27, 2024 have contraindications. • ACIP recommends high-dose inactivated (HD-IIV3) and adjuvanted inactivated (aIIV3) influenza vaccines as acceptable options for influenza vaccination of solid organ transplant recipients aged 18 through 64 years who are on immunosuppressive medication regimens, without a preference over other age-appropriate IIV3s or RIV3. Vaxelis (DTaP-IPV-Hib-HepB) • ACIP recommends DTaP-IPV-Hib-HepB (Vaxelis®) should be included with PRP-OMP (PedvaxHIB®) in the preferential recommendation June 26, 2024 for American Indian and Alaska Native infants based on the Haemophilus influenzae type b (Hib) component. *The effective date is the date when the CDC director adopted the recommendation and when the ACIP recommendation became official.